This guideline has now been superseeded by the 2015 intubation guidelines click here
Strategy for intubation by direct laryngoscopy, no predicted airway problem, no risk of regurgitation
Each step of the guideline is described.
At preoperative evaluation the anaesthetist has decided that tracheal intubation is the correct way of protecting/maintaining the airway, and has not predicted any significant problems with either direct laryngoscopy or mask ventilation. There is no increased risk of aspiration of gastro-oesophageal contents.
Airway evaluation is not perfect and problems may arise even if the patient is evaluated as not presenting airway difficulties. Strategy must cope with unexpected difficult direct laryngoscopy.
DAS suggests that this guideline represents the default strategy for intubation when this is not predicted to be difficult. The strategy deals with unexpected failed direct laryngoscopy.
The patient is anaesthetised, paralysed (usually with non-depolarising relaxants) and intubation is attempted by direct laryngoscopy.
(Please note that the quality of guideline image is low to aid fast loading. The pdf file download is good quality.)
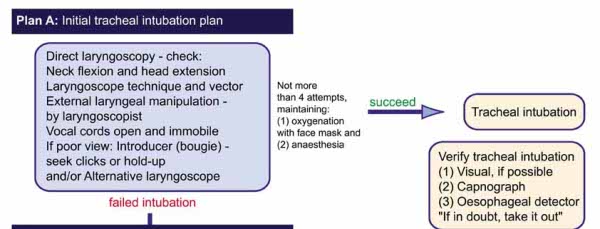
PLAN A
This is the planned first method of intubation by direct laryngoscopy.
Notes:
Intubation is attempted by optimal direct laryngoscopy and this has 5 components;
- optimal head and neck positioning
- optimal muscle relaxation
- optimal laryngoscope blade
- optimal external laryngeal manipulation
- optimal use of the bougie
A number of intubation attempts may be undertaken - to change the blade (long, straight McCoy etc), to use the bougie or to apply optimal external laryngeal manipulation. After 3-4 attempts at intubation, it is likely that the practitioner is repeating fruitless attempts and no further attempts should be made.
Correct positioning of the tube in the trachea (rather than oesophagus) should always be verified after intubation preferably by two out of the 3 best techniques of visual confirmation of the tube passing through the glottic aperture, six consecutive normal capnograph traces and inflation of the oesophageal detector device. No anaesthetist in the UK is ever expected to anaesthetise without using a working capnograph.
It is a deliberate act to stop attempts at direct laryngoscopy, announcing to your assistant 'Failed direct laryngoscopy'. This stops you having yet another attempt and alerts your assistant that you will be going on to Plan B. Start facemask ventilation and ask for a laryngeal mask. Ask for assistance. Go to plan B.
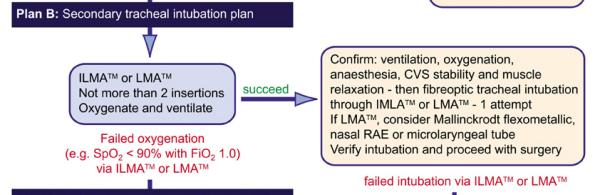
PLAN B
 Notes:
Plan B is initiated by ventilation of the patient initially by facemask and then by laryngeal mask. The laryngeal mask is particularly important and is the link between Plan A and Plan B. The priority is oxygenation and stabilising the patient - not intubation.
If ventilation is not possible by facemask or laryngeal mask go to PLAN C.
The importance of the laryngeal mask is that it generally allows;
Notes:
Plan B is initiated by ventilation of the patient initially by facemask and then by laryngeal mask. The laryngeal mask is particularly important and is the link between Plan A and Plan B. The priority is oxygenation and stabilising the patient - not intubation.
If ventilation is not possible by facemask or laryngeal mask go to PLAN C.
The importance of the laryngeal mask is that it generally allows;
- good ventilation
- attachment to the breathing system
- attachment of monitoring to display end-tidal volatile agent, oxygen and carbon dioxide levels
- provides a route for intubation
- check that the patient is oxygenated
- check that the patient is anaesthetised
- check that the patient is properly paralysed
- check that the cardiovascular sytem is stable
- check that the CO2 is at a reasonable level.
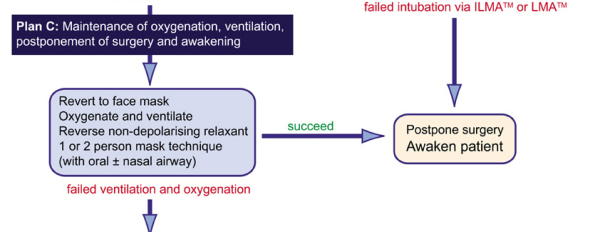 Notes:
If the LM or ILMA has been tried unsuccessfully for intubation (i.e it has been used to ventilate the patient in Plan B but intubation has not been successful) leave the device in situ, keep the patient anaesthetised and ventilated and allow the patient to wake up when muscle relaxation can be antagonised. Surgery is to be postponed and rescheduled. Awake intubation should be considered.
If at the initiation of Plan B, ventilation by laryngeal mask has not been possible (or not very satisfactory) then Plan B is bypassed to plan C. Remove the laryngeal mask if there is unsatisfactory ventilation through it and return to facemask ventilation with a large oral airway. Consider using both hands to hold the facemask with another set of hands squeezing the bag. If this fails, consider 4-handed mask ventilation in which four hands are used to apply the facemask and open the airway by jaw thrust and neck extension, with another pair of hands squeezing the bag.
If it is not possible to maintain oxygen saturations above 90% with 100% oxygen and facemask ventilation, this is a situation of Failed Ventilation and Failed Intubation and Plan D is adopted.
Notes:
If the LM or ILMA has been tried unsuccessfully for intubation (i.e it has been used to ventilate the patient in Plan B but intubation has not been successful) leave the device in situ, keep the patient anaesthetised and ventilated and allow the patient to wake up when muscle relaxation can be antagonised. Surgery is to be postponed and rescheduled. Awake intubation should be considered.
If at the initiation of Plan B, ventilation by laryngeal mask has not been possible (or not very satisfactory) then Plan B is bypassed to plan C. Remove the laryngeal mask if there is unsatisfactory ventilation through it and return to facemask ventilation with a large oral airway. Consider using both hands to hold the facemask with another set of hands squeezing the bag. If this fails, consider 4-handed mask ventilation in which four hands are used to apply the facemask and open the airway by jaw thrust and neck extension, with another pair of hands squeezing the bag.
If it is not possible to maintain oxygen saturations above 90% with 100% oxygen and facemask ventilation, this is a situation of Failed Ventilation and Failed Intubation and Plan D is adopted.
PLAN D
 Plan D is covered in another guideline.
Plan D is covered in another guideline.
